Vitamin D: How Genes Impact its Absorption and Function

Table of Contents
Vitamin D is a fat-soluble vitamin that is essential for maintaining optimal health. It is also known as the “sunshine vitamin” because the body produces it naturally when the skin is exposed to sunlight.
There are two main types of Vitamin D: Vitamin D2 (ergocalciferol), which is obtained from plant sources, and Vitamin D3 (cholecalciferol), which is synthesized in the skin upon sun exposure and obtained from certain animal sources.
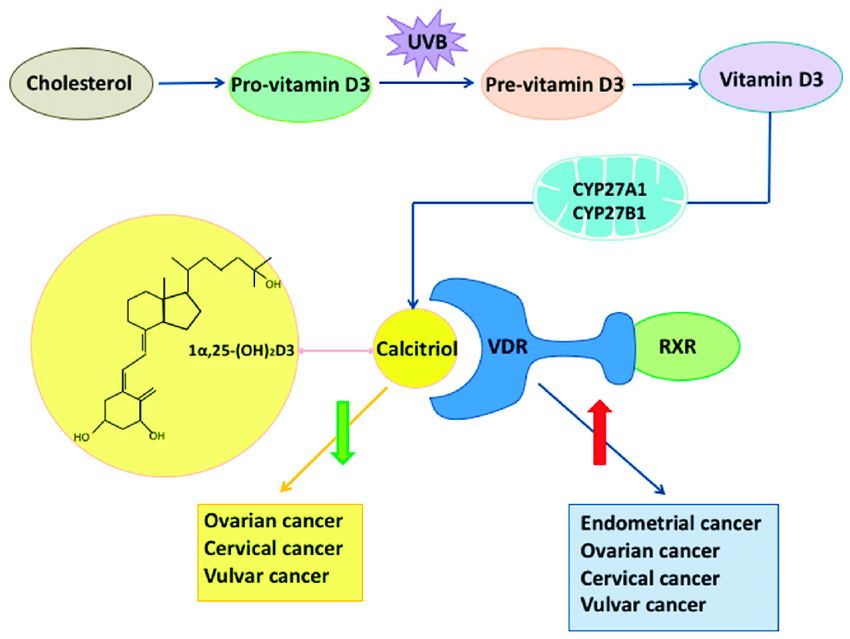
These forms of Vitamin D are biologically inert and must undergo processing (hydroxylations) in the body to get activated.
History of Vitamin D
The discovery of Vitamin D can be traced back to the early 20th century when a Polish physician, Casimir Funk, first identified vitamins.
The term “Vitamin D” was coined in 1922 during investigations into the cure for rickets, a bone disease commonly found in children.
Elmer McCollum and his associates discovered that cod liver oil, a treatment for rickets, contained not only Vitamin A (already known) but also a new compound, Vitamin D.
Over the years, further research established the pivotal role of Vitamin D in calcium metabolism and bone health.
Main functions of Vitamin D
The primary role of Vitamin D in the human body is to maintain normal calcium and phosphate levels in the blood.
It does this by aiding the absorption of calcium and phosphate from the gut, promoting bone mineralization and remodeling, and regulating the excretion of these minerals in the kidneys.
Regulation of Calcium and Phosphorus
Vitamin D is critical for the regulation of calcium and phosphorus in the body.
It aids the intestines in absorbing these minerals from the food we consume, ensuring they’re adequately used for various bodily functions.
In the absence of sufficient Vitamin D, the intestines can only absorb a fraction of these necessary minerals, which can lead to a deficiency.
When calcium levels in the blood drop, Vitamin D assists by increasing calcium absorption from the diet.
Simultaneously, it works in conjunction with the parathyroid hormone to stimulate the release of stored calcium in the bones.
This combined action helps maintain a stable level of calcium in the bloodstream, which is critical for the normal functioning of the nervous system, muscle contraction, and coagulation of blood.
Bone Health
Vitamin D plays an indispensable role in maintaining bone health.
By assisting in the absorption of calcium and phosphorus, it ensures that these minerals are available for the formation and remodeling of bones.
It is crucial for the mineralization of collagen, the protein matrix that provides structure to our bones.
Lack of sufficient Vitamin D can lead to weak or misshapen bones, as seen in the conditions of rickets in children and osteomalacia in adults.
Immune System Function
Vitamin D also contributes to the proper functioning of the immune system.
Immune cells, such as T-cells, B-cells, and antigen-presenting cells, all have Vitamin D receptors.
When activated, these cells can synthesize the active form of Vitamin D, which influences the immune response.
Emerging research suggests that Vitamin D might help modulate the immune system, enhancing the innate immune system (the body’s first line of defense) and preventing overactive immune responses, thereby reducing inflammation.
Heart Health
Recent studies have also associated Vitamin D with heart health. It may play a role in regulating blood pressure and preventing arterial damage.
Moreover, some research suggests that Vitamin D deficiency could be linked with conditions such as heart disease, stroke, and high blood pressure, though more studies are needed to confirm these findings.
Brain Function and Mental Health
Preliminary research suggests that Vitamin D might play a role in brain function and mental health.
Vitamin D receptors are present throughout the brain, including areas linked to the development of depression.
Some studies suggest a correlation between low Vitamin D levels and an increased risk of mood disorders, such as depression and anxiety, but more research is needed to fully understand these relationships.
RDA of Vitamin D
The Recommended Dietary Allowance (RDA) for Vitamin D varies with age, sex, and life stage.
For most adults aged 19-70, the RDA is 600 International Units (IU) per day, and for those aged over 70, it increases to 800 IU per day. For infants, the RDA is 400 IU per day.
However, many health professionals suggest that these recommendations may be too low, particularly for those with minimal sun exposure.
Food Sources of Vitamin D

Vegan Sources
For vegans and vegetarians, Vitamin D2 can be obtained from fortified plant-based milk, orange juice, cereals, certain types of mushrooms, and supplements.
Animal sources
Vitamin D3, which is typically better utilized by the body, is found in animal-based foods such as fatty fish (like salmon, mackerel, and sardines), fish liver oils, and egg yolks.
Some types of cheese and beef liver also contain small amounts. It’s also found in fortified dairy products and cereals.
Factors Affecting Absorption of Vitamin D
Non-Genetic Factors
Several non-genetic factors can influence Vitamin D absorption.
Sunlight exposure
Sunlight exposure is the most critical one. Latitude, altitude, time of day, season, air pollution, clothing, and sunscreen use all affect the production of Vitamin D in the skin.
Diet
Dietary factors, such as the presence of fat in the diet and the overall health of the digestive tract, also influence absorption.
Age
Aging, obesity, and skin pigmentation are other factors that can impact Vitamin D status.
Older adults, individuals with higher body fat percentages, and those with darker skin tones may require higher amounts of Vitamin D to achieve sufficient levels.
Genetic Factors
Some genetic factors can influence Vitamin D metabolism and absorption.
Variations in genes related to Vitamin D metabolism, like those involved in the synthesis of the Vitamin D receptor (VDR) and enzymes responsible for activating and deactivating Vitamin D, can affect an individual’s Vitamin D status.
In particular, several single nucleotide polymorphisms (SNPs) have been identified in genes that play significant roles in these pathways.
The following are some key genes implicated in Vitamin D metabolism:
- DHCR7/NADSYN1: These genes are involved in the production of Vitamin D3 in the skin following exposure to UVB radiation. SNPs within these genes can impact the efficiency of this process.
Check your 23andMe, Ancestry DNA raw data for DHCR7/NADSYN1 gene variants
- CYP2R1: This gene encodes an enzyme that hydroxylates Vitamin D in the liver, the first step in the activation process. Variations in this gene may influence the efficiency of this hydroxylation process, thus affecting the amount of active Vitamin D available in the body.
Check your 23andMe, Ancestry DNA raw data for CYP2R1 gene variants
- GC or DBP (Vitamin D binding protein): This gene is responsible for encoding the major carrier protein of Vitamin D, which transports it to various tissues throughout the body. SNPs in the GC gene can affect the protein’s ability to bind and transport Vitamin D.
Check your 23andMe, Ancestry DNA raw data for DBP gene variants
- CYP27B1: This gene encodes the enzyme responsible for the final activation step of Vitamin D in the kidneys. Variations in this gene can impact the body’s ability to produce the active form of Vitamin D.
Check your 23andMe, Ancestry DNA raw data for CYP27B1 gene variants
- VDR (Vitamin D Receptor): Variations in the VDR gene, which encodes the receptor to which active Vitamin D binds, can impact how effectively the body uses Vitamin D.
Check your 23andMe, Ancestry DNA raw data for VDR gene variants
Here is a table listing some of the main SNPs associated with these genes and their implications:
| Gene | SNP | Possible Implication |
|---|---|---|
| DHCR7/NADSYN1 | rs12785878 | Reduced synthesis of Vitamin D3 |
| CYP2R1 | rs10741657 | Altered hydroxylation, affecting Vitamin D levels |
| GC/DBP | rs2282679 | Altered Vitamin D transport |
| CYP27B1 | rs10877012 | Reduced conversion to active Vitamin D |
| VDR | rs2228570 (also known as FokI polymorphism) | Altered Vitamin D receptor function |
Please note that the presence of these SNPs doesn’t necessarily mean an individual will have altered Vitamin D levels or activity in the body, as these processes are influenced by various factors, including environmental and lifestyle factors.
Causes of Vitamin D Deficiency
Vitamin D deficiency can occur due to a variety of reasons, including inadequate dietary intake, limited sun exposure, malabsorption issues in the digestive system, obesity, and certain medical conditions such as kidney and liver diseases.
Some medications, including certain anti-seizure medications, glucocorticoids, and AIDS/HIV drugs, can also affect Vitamin D metabolism and lead to deficiency.
Effects of Vitamin D Deficiency
Vitamin D deficiency can lead to a variety of health issues. In children, severe deficiency can result in rickets, characterized by soft, weak, deformed bones.
In adults, deficiency can lead to
- osteomalacia (soft bones)
- osteoporosis (fragile bones)
In addition to bone health, Vitamin D deficiency may be associated with an increased risk of several chronic diseases such as cancer, autoimmune diseases, infectious diseases, and cardiovascular diseases.

What are the general symptoms of vitamin D deficiency?
- fatigue,
- muscle weakness, and
- general aches and pains.
However, many individuals with Vitamin D deficiency may not exhibit any symptoms until levels are very low or have been low for a significant period.
Summary
Vitamin D’s roles in the body are vast and varied, ranging from bone health to immune function and beyond. These various roles underscore the importance of maintaining adequate Vitamin D levels for overall health and well-being.
References
- Wang TJ, Zhang F, Richards JB, et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 2010;376(9736):180-188. doi:10.1016/S0140-6736(10)60588-0
- Ahn J, Yu K, Stolzenberg-Solomon R, et al. Genome-wide association study of circulating vitamin D levels. Hum Mol Genet. 2010;19(13):2739-2745. doi:10.1093/hmg/ddq155
- Jolliffe DA, Walton RT, Griffiths CJ, Martineau AR. Single nucleotide polymorphisms in the vitamin D pathway associating with circulating concentrations of vitamin D metabolites and non-skeletal health outcomes: Review of genetic association studies. J Steroid Biochem Mol Biol. 2016;164:18-29. doi:10.1016/j.jsbmb.2015.12.007
Written By
Share this article












