Genetics of Salt Sensitivity and Blood Pressure
Table of Contents
Symptoms Of Hypertension
Hypertension, or high blood pressure, is often referred to as a “silent killer” because it typically has no overt symptoms.
Despite this, there can be some indirect signs, including headaches, shortness of breath, dizziness, chest pain, or visual changes.
Often, hypertension is detected during routine health check-ups.
What Causes Hypertension?
The exact cause of hypertension is not known, but it is influenced by various factors including age, sex, family history, and lifestyle factors such as diet, physical activity, and smoking.
Certain medical conditions, such as kidney disease, can also contribute to the development of hypertension.
Salt Sensitivity: What the Research Says
Scientific research has made significant strides in understanding salt sensitivity and its implications for health. Here’s what we know:
- Prevalence: Studies suggest that about 51% of people with hypertension are salt-sensitive, as are 26% of people with normal blood pressure.
- Risk Factors: Research indicates that salt sensitivity is more common among older adults, African Americans, people with obesity, and those with metabolic syndrome.
- Genetics: Certain genetic variants have been associated with an increased risk of salt sensitivity, although the genetic aspect of this condition is complex and multifactorial.
- Dietary Impact: Studies show that a lower salt diet can significantly reduce blood pressure in individuals with salt sensitivity.
- Health Outcomes: Research has associated salt sensitivity with an increased risk of cardiovascular disease, kidney disease, and stroke.
- Testing: Currently, the gold standard for diagnosing salt sensitivity is a controlled dietary intervention with monitoring of blood pressure responses. However, the development of more convenient and accessible testing methods is an active area of research.
It’s important to note that while the study of salt sensitivity has come a long way, there is still much to learn.
Understanding the complex interplay between genetics, diet, and other factors that contribute to salt sensitivity could pave the way for personalized dietary recommendations and targeted therapies for managing hypertension.
As always, individuals should consult with healthcare professionals for personalized advice and treatment.
Understanding Salt Sensitivity
Salt sensitivity is a measure of how your blood pressure responds to dietary salt intake.
It’s a term that describes the relationship between the consumption of sodium (which is primarily found in salt) and changes in blood pressure levels.
For some individuals, consuming salt doesn’t lead to significant changes in their blood pressure.
These individuals are referred to as ‘salt-resistant’.
However, for others, known as ‘salt-sensitive’, even a small increase in dietary salt can lead to noticeable increases in blood pressure.
A report by the American Heart Association revealed that approximately 50% of people with hypertension (high blood pressure) and about 25% of people with normal blood pressure are salt-sensitive.
The causes of salt sensitivity are not fully understood yet.
It’s likely a complex trait influenced by many factors, including genetics, age, diet, and other lifestyle aspects.
Genetically, variations in certain genes have been associated with an increased risk of salt sensitivity, such as the ACE gene involved in regulating blood pressure.
These genetic variations can affect how the kidneys handle sodium, leading to increased blood pressure when more salt is consumed.
Non-Genetic Factors Affecting Salt-Sensitivity
From a lifestyle perspective, salt sensitivity may be influenced by diet and exercise habits.
Diets high in processed foods, which often contain large amounts of sodium, may increase the risk of salt sensitivity.
Exercise, on the other hand, has been shown to reduce blood pressure and may also influence salt sensitivity.
As salt sensitivity can increase the risk of hypertension, heart disease, and stroke, understanding whether you’re salt-sensitive and managing your salt intake can be important steps toward better health.
It’s worth noting that most people consume more salt than recommended by health organizations, so aiming for a diet low in salt is generally a healthy choice regardless of salt sensitivity status.
If you suspect you may be salt-sensitive, speak with a healthcare provider.
They may recommend changes in your diet or lifestyle and can provide guidance based on your personal health history and needs.
Remember that even small changes can have a significant impact on your overall health and well-being.
How To Determine If You Are Salt Sensitive?
Determining salt sensitivity usually requires a clinical evaluation, which may include a dietary intervention with different levels of salt intake and monitoring blood pressure responses.
It’s important to consult with a healthcare provider for an accurate diagnosis.
Genetics, Salt, and Blood Pressure
The genetic component of salt sensitivity and hypertension is multifaceted and is influenced by numerous genes that interact with each other and with environmental factors.
ACE Gene
One key gene of interest is the aforementioned ACE (Angiotensin-Converting Enzyme) gene.
Variations in the ACE gene can impact the activity of the enzyme it codes for, affecting the balance of hormones that regulate blood pressure and the body’s response to dietary salt.
Some variants have been associated with higher enzyme activity, potentially leading to higher blood pressure in the presence of high dietary salt.
Check your AncestryDNA, 23andMe raw data for the ACE gene variants
AGT Gene
Another important gene is AGT (Angiotensinogen).
This gene provides instructions for making a protein called angiotensinogen, which is the precursor to angiotensin II, a powerful vasoconstrictor that plays a central role in blood pressure regulation.
Certain variants in the AGT gene can lead to increased production of angiotensinogen, potentially contributing to higher blood pressure and salt sensitivity.
Check your AncestryDNA, 23andMe raw data for the AGT gene variants
ADD1 Gene
The ADD1 (Adducin 1) gene also plays a role in blood pressure regulation and salt sensitivity.
Adducin is a protein that helps regulate the transport of sodium (salt) into cells.
Certain variants in the ADD1 gene have been associated with an increased risk of hypertension and greater blood pressure response to dietary salt.
Check your AncestryDNA, 23andMe raw data for the ADD1 gene variants
CYP11B2 Gene
Additionally, variations in the CYP11B2 (Aldosterone synthase) gene, which is involved in the production of the hormone aldosterone, can influence the body’s response to salt and impact blood pressure levels.
Check your AncestryDNA, 23andMe raw data for the CYP11B2 gene variants
More on the ACE Gene’s Role in Blood Pressure Control
The ACE gene, standing for Angiotensin-Converting Enzyme, plays a crucial role in maintaining blood pressure homeostasis in our bodies.
It does so by participating in the Renin-Angiotensin System (RAS), a hormone system that regulates blood pressure and fluid balance.
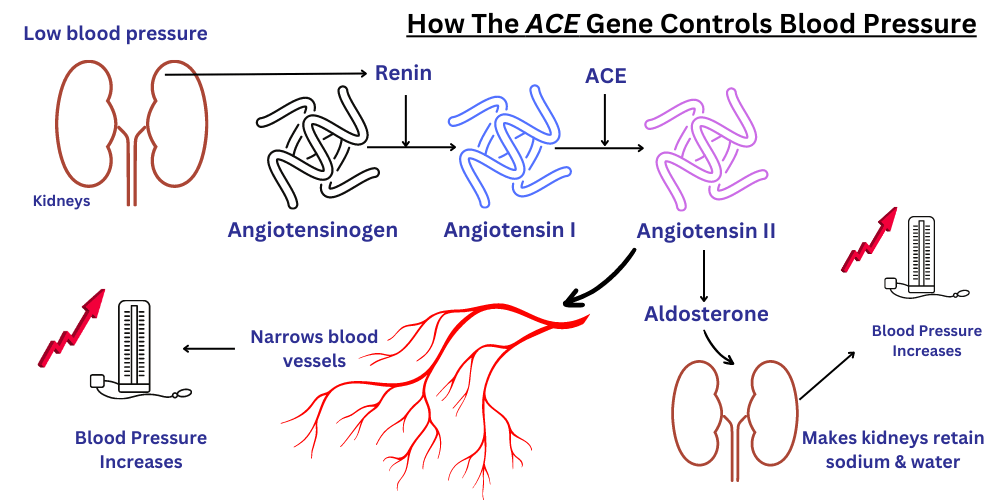
Here’s how it works at the molecular level:
- Renin: When blood pressure is low, the kidneys produce renin, an enzyme that initiates a series of reactions.
- Angiotensinogen to Angiotensin I: Renin acts on a protein in the blood called angiotensinogen, converting it into angiotensin I.
- Angiotensin I to Angiotensin II: Here’s where the ACE gene comes into play. The ACE gene provides instructions for making an angiotensin-converting enzyme, which converts angiotensin I into angiotensin II.
- Angiotensin II: This molecule is a potent vasoconstrictor, meaning it narrows blood vessels, thereby increasing blood pressure. It also stimulates the release of another hormone called aldosterone.
- Aldosterone: This hormone prompts the kidneys to retain sodium and water, which also helps to increase blood pressure.
A variant in the ACE gene can impact the levels or activity of the angiotensin-converting enzyme, which may affect blood pressure regulation and contribute to salt sensitivity.
In particular, some variants have been associated with higher enzyme activity, leading to increased levels of angiotensin II and potentially higher blood pressure, especially in the context of high dietary salt intake.
| SNP ID | Location | Description | Possible Influence on Blood Pressure |
|---|---|---|---|
| rs4291 | Promoter region | Influences ACE gene transcription | May impact hypertension risk, but studies vary |
| rs4343 | Coding region | Synonymous mutation | Association with hypertension observed in multiple populations |
| rs4362 | Coding region | N/A | Some studies suggest a significant association with blood pressure regulation |
| rs1799752 (ACE I/D) | Intronic region | Indel polymorphism resulting in presence (I) or absence (D) of a 287 bp Alu repeat | Indel polymorphism resulting in the presence (I) or absence (D) of a 287 bp Alu repeat |
Please remember, the actual influence of these SNPs on your health may depend on various factors including your overall genetic makeup, environment, and lifestyle. Always consult with a healthcare provider for personal medical advice.
Section Summary
These are just a few of the genes involved in salt sensitivity and blood pressure regulation.
In reality, it’s likely that many more genes play a role, each contributing a small part to an individual’s overall risk.
This makes the genetic aspect of salt sensitivity a complex trait, influenced by the interaction of multiple genes and environmental factors.
It’s important to note that while we have made significant strides in understanding the genetic aspects of salt sensitivity and blood pressure regulation, there is still much to learn.
Ongoing research continues to uncover new genes and molecular mechanisms involved in these processes, which will hopefully lead to improved methods for predicting, diagnosing, and treating hypertension in the future.
Eating Right as a Salt-Sensitive Individual
If you’re sensitive to salt, a small adjustment to your dietary habits can have a big impact on your overall health, especially your blood pressure.
Here are some tips to help you manage your salt intake:
- Read Labels: Packaged and processed foods often contain high levels of sodium. Always read nutrition labels to check the sodium content. Foods that contain less than 5% of the daily value of sodium can be considered low in sodium.
- Cook at Home: One of the easiest ways to control your salt intake is to cook your own meals. This way, you’re in control of how much salt is added to your food.
- Spice It Up: Instead of relying on salt for flavor, try using other seasonings like herbs, spices, vinegar, or lemon juice. There’s a wide variety of spices that can make your meals flavorful without increasing your sodium intake.
- Increase Potassium Intake: Foods rich in potassium can help counteract the effects of sodium on blood pressure. Include foods like bananas, oranges, spinach, sweet potatoes, and avocados in your diet.
- Choose Fresh Foods: Fresh fruits and vegetables are naturally low in sodium. Likewise, fresh meats are lower in sodium than deli meats or sausages.
- Limit Eating Out: Restaurant meals can be high in sodium, especially fast food. If you do eat out, don’t hesitate to ask for your meal to be prepared with less salt.
- Reduce Portion Sizes: If reducing the salt in your favorite meals makes them less enjoyable, try eating smaller portions instead. This will reduce your overall sodium intake.
- Stay Hydrated: Drinking plenty of water can help your body manage sodium and maintain healthy blood pressure.
- Gradual Changes: If you’re used to eating a lot of salt, it might take a while for your taste buds to adjust to less salty foods. Start by gradually decreasing the amount of salt you add to your food and you’ll eventually come to enjoy foods with less sodium.
Remember, everyone’s body responds differently to dietary changes, so it’s important to monitor your blood pressure and work with your healthcare provider to find a dietary plan that works for you.
Summary
Understanding the interplay between hypertension, salt sensitivity, and genetic factors can provide valuable insights for managing blood pressure. Eating a balanced, low-sodium diet and maintaining a healthy lifestyle is essential for blood pressure control.
Cited Works
- Svetkey, L. P., McKeown, S. P., & Wilson, A. F. (1996). Heritability of salt sensitivity in black Americans. Hypertension, 28(5), 854-858.
- Weinberger, M. H. (1996). Salt sensitivity of blood pressure in humans. Hypertension, 27(3 Pt 2), 481-490.
- Meneton, P., Jeunemaitre, X., de Wardener, H. E., & MacGregor, G. A. (2005). Links between dietary salt intake, renal salt handling, blood pressure, and cardiovascular diseases. Physiological reviews, 85(2), 679-715.
- Sharma, A. M., & Cetto, C. (1992). The adipose tissue in the pathogenesis of salt-sensitive hypertension. Klinische Wochenschrift, 70(11), 1254-1258.
- Rapp, J. P. (1982). Genetic analysis of inherited hypertension in the rat. Physiological reviews, 62(1), 59-128.
- Beeks, E., Kessels, A. G., Kroon, A. A., van der Klauw, M. M., & de Leeuw, P. W. (2004). Genetic predisposition to salt-sensitivity: a systematic review. Journal of hypertension, 22(7), 1243-1249.
- Ji, W., Foo, J. N., O’Roak, B. J., Zhao, H., Larson, M. G., Simon, D. B., … & Lifton, R. P. (2008). Rare independent mutations in renal salt handling genes contribute to blood pressure variation. Nature Genetics, 40(5), 592-599.
Written By
Share this article












