Insulin Sensitivity: Decoding The Genetic Factors

Table of Contents
What is Insulin Sensitivity?
Insulin sensitivity refers to how responsive your cells are to insulin.
In simple terms, if you are insulin sensitive, your cells will use insulin efficiently, helping to regulate blood glucose levels properly.
When you eat, your blood glucose levels rise, triggering your pancreas to release insulin. This hormone helps your cells take in glucose and use it for energy or store it for later use.
Is Insulin Sensitivity Good?
Yes, having a high level of insulin sensitivity is beneficial.
It means your body needs less insulin to lower blood glucose levels, which helps maintain overall metabolic health.
Low insulin sensitivity, also known as insulin resistance, is associated with several health issues, including obesity, heart disease, and type 2 diabetes.
How to Improve Insulin Sensitivity?
Improving insulin sensitivity is primarily a function of lifestyle changes. Here are some key strategies:
- Exercise regularly: Physical activity helps muscle cells use blood glucose for energy, increasing insulin sensitivity.
- Maintain a healthy weight: Overweight and obesity are linked with insulin resistance. Achieving and maintaining a healthy weight can significantly improve insulin sensitivity.
- Eat a healthy diet: A diet rich in whole grains, lean proteins, fruits, vegetables, and healthy fats can improve insulin sensitivity.
What is the Insulin Sensitivity Factor?
The insulin sensitivity factor, also known as the insulin-to-carb ratio or correction factor, is an estimate of how much one unit of insulin will reduce a person’s blood glucose level.
It’s particularly important for people with diabetes who use insulin therapy to manage their blood glucose levels.
Non-Genetic Factors Affecting Insulin Sensitivity
Does exercise increase insulin sensitivity?
Yes, exercise can significantly increase insulin sensitivity.
Physical activity promotes increased uptake of glucose into cells, decreasing blood glucose levels.
Both aerobic exercise (like running or biking) and resistance training (like weight lifting) can increase insulin sensitivity.
Does fasting improve insulin sensitivity?
Emerging research suggests that intermittent fasting, where one alternate between periods of eating and fasting, may improve insulin sensitivity.
However, the full effects of fasting on insulin sensitivity are complex and depend on factors like the duration and frequency of fasting periods, overall diet, and individual health status.
Does metformin improve insulin sensitivity?
Metformin, a common medication prescribed for type 2 diabetes, works by improving insulin sensitivity.
It reduces the amount of glucose your liver produces and makes your body’s cells more responsive to insulin.
Does walking improve insulin sensitivity?
Yes, walking can improve insulin sensitivity. Regular walking, especially after meals, can help reduce post-meal blood sugar spikes and improve overall insulin response.
Does alcohol affect insulin sensitivity?
Alcohol can both increase and decrease insulin sensitivity, depending on the amount consumed and individual characteristics.
Moderate alcohol consumption has been associated with increased insulin sensitivity, but excessive alcohol consumption can have the opposite effect and lead to decreased insulin sensitivity.
Can caffeine affect insulin sensitivity?
Caffeine has been shown to decrease insulin sensitivity in the short term.
However, the long-term effects of caffeine on insulin sensitivity are less clear, and some studies suggest that regular coffee drinkers might have improved insulin sensitivity.
Can Insulin Sensitivity Be Reversed?
Insulin resistance, the opposite of insulin sensitivity, can often be reversed or significantly improved through lifestyle changes.
Regular exercise, a balanced diet, weight loss, and medications such as metformin can all contribute to improved insulin sensitivity.
Genes influencing insulin sensitivity
Certain genes, such as those involved in glucose metabolism, insulin signaling, and inflammation, can influence insulin sensitivity.
Genetic variants in these genes might contribute to individual differences in insulin sensitivity and the risk of developing conditions like type 2 diabetes.
TCF7L2
Transcription factor 7-like 2 (TCF7L2) is a gene that is predominantly associated with type 2 diabetes, the most common form of diabetes characterized by insulin resistance.
This gene is involved in the Wnt signaling pathway, which plays a role in many biological processes, including the regulation of glucose metabolism.
Fascinating Facts: Wnt signalling pathway is highly favoured by evolution. Hence its found across animal species from fruti flies to humans
Several studies have reported that specific variants in the TCF7L2 gene can increase the risk of developing type 2 diabetes.
While the exact mechanisms are still being explored, it’s suggested that these variants may impair the body’s ability to secrete insulin in response to rising blood glucose levels, contributing to decreased insulin sensitivity.
PPARG
Peroxisome Proliferator-Activated Receptor Gamma (PPARG) is a gene involved in regulating fatty acid storage and glucose metabolism.
The protein produced by this gene is found in fat tissue and plays a vital role in adipogenesis, the process of forming new fat cells.
Certain variations in the PPARG gene are associated with increased susceptibility to insulin resistance, particularly in individuals who are obese.
These variants may alter the function of the PPARG protein, disrupting the normal regulation of fatty acid storage and glucose metabolism, and leading to reduced insulin sensitivity.
IRS1
The Insulin Receptor Substrate 1 (IRS1) gene plays a critical role in the insulin signaling pathway.
This gene produces a protein that spreads the signal from the insulin receptor located on the cell’s surface into the cell after insulin binds to it.
This signal triggers various processes that enable cells to take up glucose from the bloodstream and use it for energy.
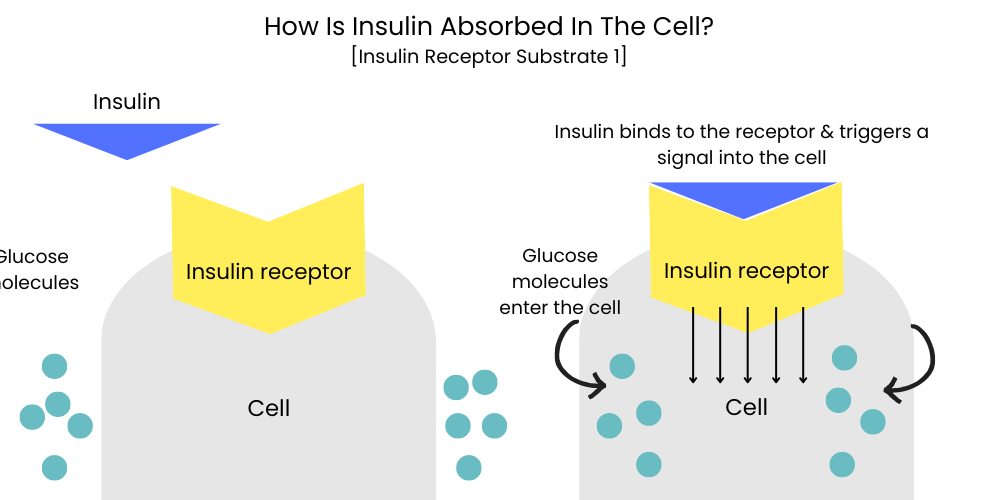
Disruptions or variations in the IRS1 gene can impair insulin signal transduction, meaning that even when insulin is present, the signal to take up glucose might not be adequately passed on, leading to insulin resistance.
KCNJ11
The KCNJ11 gene encodes a protein that forms a key part of a potassium channel in the beta cells of the pancreas.
This channel plays a critical role in insulin secretion by regulating the electrical activity of beta cells.
Variants of this gene may affect the functioning of the potassium channel, thereby influencing insulin secretion.
Impaired insulin secretion can, in turn, affect insulin sensitivity and glucose homeostasis, increasing the risk of type 2 diabetes.
Which KCNJ11 gene variants do you have? Check your Ancestry DNA, 23andMe raw data
ADIPOQ
The ADIPOQ gene encodes the protein hormone adiponectin, produced and secreted by adipose tissue.
Adiponectin enhances insulin sensitivity and has anti-inflammatory effects.
It improves the body’s ability to properly respond to insulin by increasing the metabolism of fatty acids and enhancing glucose uptake by cells.
Certain variants in the ADIPOQ gene can lead to reduced adiponectin levels, which may result in decreased insulin sensitivity.
Lower adiponectin levels have been observed in individuals with obesity and insulin resistance, suggesting a potential link between ADIPOQ variants and these conditions.
Which ADIPOQ gene variants do you have? Check your Ancestry DNA, 23andMe raw data
FTO
The FTO gene, often associated with obesity, can also influence insulin sensitivity indirectly.
Variants of this gene have been linked to increased body mass index (BMI) and alterations in body composition, which may affect insulin sensitivity. Increased fat mass, particularly visceral fat, is associated with insulin resistance.
Which FTO gene variants do you have? Check your Ancestry DNA, 23andMe raw data
GLUT4
The GLUT4 gene provides instructions for making a glucose transporter protein that plays a critical role in insulin-stimulated glucose uptake into cells, particularly in muscle and fat tissues.
When insulin binds to its receptor, it triggers a series of events that lead to the movement of GLUT4 from inside the cell to the cell’s surface, allowing glucose to enter the cell.
Variants in this gene might reduce GLUT4‘s activity, limiting the capacity of insulin to stimulate glucose uptake into cells.
This can lead to higher levels.
Which GLUT4 gene variants do you have? Check your Ancestry DNA, 23andMe raw data
Improve Your Insulin Sensitivity: Exercise for your Genes
Designing a fitness routine to improve insulin sensitivity based on your genes first requires understanding your genetic profile.
A healthcare professional or genetic counselor with knowledge of genomics can provide this information.
Several companies offer genetic testing kits that can offer insight into your health and fitness characteristics.
It’s important to remember, though, that genetic results are not deterministic and should not be used in isolation for health decisions.
For instance, variants in certain genes might indicate that you’d benefit more from resistance training or aerobic exercises. The following are some examples:
Aerobic Exercises – FTO Gene
Individuals with variants in the FTO gene are often at a higher risk of obesity and insulin resistance.
Studies have shown that regular aerobic exercises like cycling, jogging, or swimming can significantly improve insulin sensitivity in these individuals, even without weight loss.
Week 1-2:
- Start with moderate-intensity workouts like brisk walking or cycling at a relaxed pace for 20-30 minutes a day, three times a week.
Week 3-4:
- Gradually increase your workout time to 30-45 minutes per session, still focusing on moderate-intensity aerobic exercises.
Week 5 onwards:
- Incorporate higher-intensity aerobic exercises like jogging, swimming, or cycling at a brisk pace. Aim to work out for at least 45 minutes a day, five times a week.
Resistance Training – IRS1 Gene
Variants in the IRS1 gene can impair insulin signaling.
Resistance training can be particularly effective for individuals with this genetic variant, as it increases muscle mass, which aids in glucose uptake.
Week 1-2:
- Start with simple strength training exercises using your body weight, like push-ups, squats, or lunges. Begin with one set of 10-12 repetitions for each exercise, three times a week.
Week 3-4:
- Add more exercises to your routine and start using light weights. Increase to two sets of 10-12 repetitions for each exercise.
Week 5 onwards:
- Gradually increase the weights you’re using and consider adding more resistance exercises. Aim to do strength training workouts for at least 30 minutes, three to four times a week.
Remember, any exercise is better than no exercise.
So even if your genes indicate you might benefit more from one type of exercise, it’s important to choose activities that you enjoy.
This will help you stick with your workout routine in the long term.
Always consult a healthcare professional before starting a new workout routine, especially if you have any pre-existing health conditions.
Improve Your Insulin Sensitivity: Eat for your Genes
Designing a diet to improve insulin sensitivity based on your genes requires understanding your unique genetic profile.
A dietician or a healthcare professional with expertise in genomics can provide personalized advice based on your genetic results.
Many direct-to-consumer genetic testing kits offer insights into how your body might respond to different nutrients, but it’s crucial to remember these results should not be used in isolation for dietary decisions.
Let’s consider a few examples:
High Fiber Diet – TCF7L2 Gene
Variants in the TCF7L2 gene have been associated with a greater risk of type 2 diabetes.
Individuals with these genetic variants might benefit from a diet high in fiber, as it can help regulate blood glucose levels and improve insulin sensitivity.
Dietary Plan:
- Incorporate a variety of high-fiber foods in your meals like fruits, vegetables, whole grains, and legumes.
- Choose breakfast cereals that are whole grain and rich in fiber.
- Opt for whole grain or multi-grain bread for sandwiches.
- Include a side of vegetables or a salad in your lunch and dinner.
- Make fruits your go-to for snacks.
Which TCF7L2 gene variants do you have? Check your Ancestry DNA, 23andMe raw data
Low Saturated Fat Diet – PPARG Gene
Certain variants in the PPARG gene can make individuals more susceptible to insulin resistance, especially in the context of a diet high in saturated fat.
A diet low in saturated fats and high in mono and polyunsaturated fats could be beneficial.
Dietary Plan:
- Limit intake of high-fat meat products and full-fat dairy products, which are high in saturated fats.
- Include sources of good fats in your diet, like avocados, fatty fish, nuts, and seeds.
- Cook with oils that are high in unsaturated fats, like olive oil or canola oil.
- Avoid processed foods and fast foods, which often contain a high amount of saturated and trans fats.
Which PPARG gene variants do you have? Check your Ancestry DNA, 23andMe raw data
Balanced Carbohydrate Intake – GLUT4 Gene
Individuals with certain variants in the GLUT4 gene might have reduced glucose uptake into cells.
These individuals might benefit from a diet with a balanced and consistent carbohydrate intake, spread throughout the day, to prevent spikes in blood glucose levels.
Dietary Plan:
- Aim for consistent carbohydrate intake at each meal.
- Incorporate complex carbohydrates, like whole grains and legumes, that are slowly digested and released into the bloodstream.
- Limit high-glycemic foods that can cause rapid spikes in blood sugar, like sugary drinks, white bread, and pastries.
- Consider pairing carbohydrates with protein or healthy fats, which can slow down the release of glucose into the bloodstream.
Omega-3 Rich Diet – LIPC Gene
The LIPC gene plays a role in the breakdown of fats in the body.
Certain variants of the LIPC gene can affect HDL (“good”) cholesterol levels, and there’s some evidence that these variants may also influence insulin sensitivity.
Consuming a diet rich in omega-3 fatty acids, which are known to increase HDL cholesterol levels, might be beneficial for individuals with these genetic variants.
Dietary Plan:
- Increase consumption of fatty fish like salmon, mackerel, and sardines, which are high in omega-3 fatty acids.
- Include walnuts, flaxseeds, and chia seeds in your diet, which are plant-based sources of omega-3s.
- Consider using canola oil or flaxseed oil for cooking, as these oils are rich in omega-3s.
- If it’s difficult to get enough omega-3s through your diet, discuss with your healthcare provider about the possibility of taking omega-3 supplements.
Which LIPC gene variants do you have? Check your Ancestry DNA, 23andMe raw data
Anti-Inflammatory Diet – CRP Gene
The CRP gene is involved in the production of C-reactive protein, a marker of inflammation in the body.
High levels of C-reactive protein indicates that there is a lot of inflammation in your body. This has been linked to a higher risk of insulin resistance.
An anti-inflammatory diet could be beneficial for individuals with certain variants in the CRP gene.
Dietary Plan:
- Consume a variety of fruits and vegetables, which are rich in antioxidants that can help reduce inflammation.
- Choose whole grains over refined grains, as they have higher levels of nutrients and fiber that can help regulate blood sugar levels.
- Include sources of omega-3 fatty acids, like fatty fish and walnuts, which have anti-inflammatory properties.
- Limit consumption of processed foods and beverages high in sugar, as these can increase inflammation.
- Use spices and herbs, like turmeric and ginger, known for their anti-inflammatory properties, in your cooking.
It’s important to remember that while these dietary strategies are based on your genetic predisposition, they should be part of a balanced diet that considers your overall health, lifestyle, and food preferences.
Always consult with a healthcare provider or a dietitian before making significant changes to your diet.
Summarize in the form of FAQs
Q: What is insulin sensitivity? A: It’s how responsive your cells are to insulin, a hormone that regulates blood glucose levels.
Q: Is insulin sensitivity good? A: Yes, high insulin sensitivity is beneficial as it helps maintain overall metabolic health.
Q: How can I improve my insulin sensitivity? A: Regular exercise, a balanced diet, maintaining a healthy weight, getting enough sleep, and managing stress effectively can all improve insulin sensitivity.
Q: Does exercise increase insulin sensitivity? A: Yes, both aerobic exercise and resistance training can increase insulin sensitivity.
Q: Can insulin resistance be reversed? A: Yes, lifestyle changes and certain medications can often reverse or significantly improve insulin resistance.
Q: How do genes influence insulin sensitivity? A: Certain genes involved in glucose metabolism, insulin signaling, and inflammation can influence insulin sensitivity.
References
- Kahn, B. B., & Flier, J. S. (2000). Obesity and insulin resistance. Journal of Clinical Investigation, 106(4), 473–481.
- Sigal, R. J., Kenny, G. P., Wasserman, D. H., Castaneda-Sceppa, C., & White, R. D. (2006). Physical Activity/Exercise and Type 2 Diabetes. Diabetes Care, 29(6), 1433–1438.
- Harvard Health Publishing. (2020). The sweet danger of sugar. Harvard Medical School.
- Inzucchi, S. E., Bergenstal, R. M., Buse, J. B., Diamant, M., Ferrannini, E., Nauck, M., & Matthews, D. R. (2015). Management of Hyperglycemia in Type 2 Diabetes, 2015: A Patient-Centered Approach. Diabetes Care, 38(1), 140–149.
- Centers for Disease Control and Prevention. (2020). Diabetes and Your Lifestyle: Eating, Exercise, and Weight Loss.
- Templeman, N. M., Skovsø, S., Page, M. M., Lim, G. E., & Johnson, J. D. (2017). A causal role for hyperinsulinemia in obesity. Journal of Endocrinology, 232(3), R173–R183.
Written By
Share this article












