Achilles Tendinopathy: Effective Therapy and Influential Genetics

Table of Contents
What is Achilles Tendinopathy?
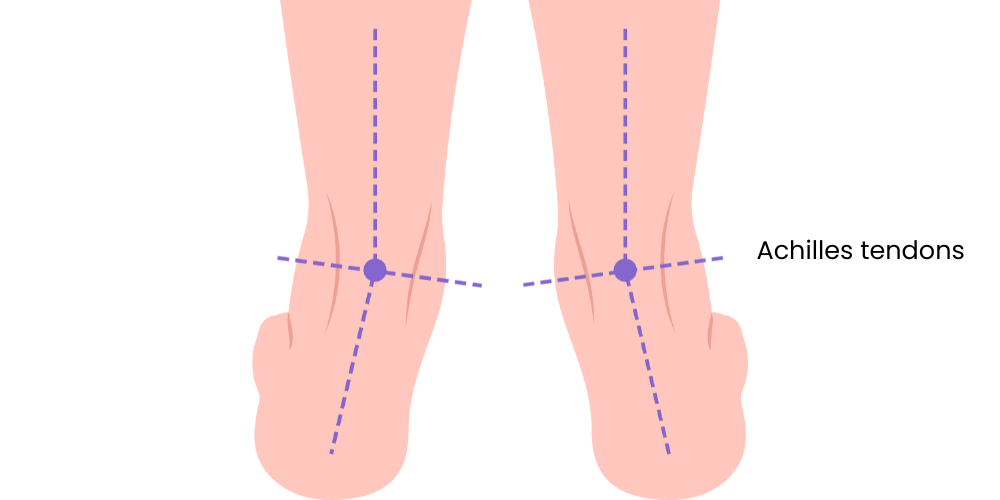
Achilles tendinopathy is a condition that affects the Achilles tendon, the largest and strongest tendon in the human body.
The Achilles tendon is responsible for connecting the calf muscles to the heel bone.
The condition is characterized by pain, swelling, and reduced function, and is often caused by overuse or repetitive strain.
Two types of Achilles tendinopathy exist:
- non-insertional (involving the middle portion of the tendon)
- insertional (involving the lower portion where the tendon attaches to the heel bone).
Can You Run with Achilles Tendinopathy?
While it is possible to run with Achilles tendinopathy, it is not advisable without proper medical consultation.
Running can exacerbate the injury, leading to increased pain and potentially more severe complications.
If you are an athlete or someone who regularly runs, it is crucial to seek professional medical advice before continuing your usual running regimen.
How Do You Treat Achilles Tendinopathy?
The treatment of Achilles tendinopathy typically involves a multi-modal approach that includes rest, ice, compression, and elevation (RICE), alongside pain management with non-steroidal anti-inflammatory drugs (NSAIDs).
Additionally, physiotherapy plays a key role in treatment.
Exercises to strengthen the calf muscles and improve flexibility can aid recovery, and in some cases, orthotic devices may be recommended.
In severe cases, where conservative treatment fails, surgical intervention may be necessary.
How Long Does Achilles Tendinopathy Take to Heal?
The healing time for Achilles tendinopathy varies greatly and is dependent on the severity of the condition and the individual’s overall health.
Typically, minor cases can resolve within a few weeks to a few months of appropriate treatment.
However, more severe or chronic cases may require several months or even longer to fully recover.
How to Cure Achilles Tendinopathy?
As stated earlier, curing Achilles tendinopathy involves a combination of rest, physiotherapy, and potentially surgical intervention in severe cases.
Additionally, modifications to footwear and running techniques can help prevent future recurrence.
What Causes Achilles Tendinopathy?
The main cause of Achilles tendinopathy is overuse or repetitive strain on the Achilles tendon.
This is often seen in athletes or individuals who participate in high-impact activities.
Other factors include improper footwear, a sudden increase in activity level, and biomechanical problems like flat feet or overpronation.
Genes Influencing Achilles Tendinopathy
The development of Achilles tendinopathy is believed to be multifactorial, involving a combination of environmental and genetic factors.
Several gene variations have been implicated in the increased risk of developing Achilles tendinopathy.
COL5A1 gene
One of the most notable genetic factors is the COL5A1 gene.
This gene is responsible for the production of type V collagen, an essential component of the tendons and ligaments.
Variants of the COL5A1 gene have been associated with an altered structure and function of the tendon, leading to a higher susceptibility to injuries like Achilles tendinopathy.
MMP3 gene
Another gene of interest is the MMP3 gene, which encodes a matrix metalloproteinase enzyme involved in the degradation of the extracellular matrix in normal physiological processes, such as tissue remodeling and wound healing.
Variants of the MMP3 gene might affect the stability and flexibility of the tendon, potentially leading to Achilles tendinopathy.
TNC gene
The TNC gene, encoding the protein tenascin-C, is also believed to play a role in Achilles tendinopathy.
This protein is involved in tissue injury responses and can influence tendon healing.
Variations in the TNC gene could impact the tendon’s ability to recover from injury, contributing to the development of tendinopathy.
GDF5 gene
The GDF5 gene, encoding growth differentiation factor 5, has also been implicated in tendon injuries.
This gene plays a crucial role in the development and repair of bone and cartilage, and variants of this gene might affect tendon health and recovery.
IL-1β gene
Lastly, the IL-1β gene, involved in inflammatory responses, has been associated with chronic tendon disorders.
Variations in this gene can influence the level of inflammation in response to tendon injury, potentially contributing to the development and persistence of Achilles tendinopathy.
Section Summary
It’s important to note that genetic factors alone are not responsible for Achilles tendinopathy.
Rather, they interact with environmental and lifestyle factors, such as physical activity levels, footwear, and biomechanics, to influence an individual’s risk of developing the condition.
Non-Genetic Factors Influencing Achilles Tendinopathy
While genetics play a role in the susceptibility to Achilles tendinopathy, various non-genetic factors can also influence the development of this condition.
These can be divided into lifestyle factors, biomechanical factors, and medical factors.
Lifestyle Factors
Physical Activity
The level and type of physical activity significantly influence the risk of Achilles tendinopathy.
High-impact activities and sports that involve running, jumping, or sudden changes in direction put a significant strain on the Achilles tendon, leading to an increased risk of injury.
Training Regimen
How an individual trains also plays a role.
A sudden increase in training intensity or volume, inadequate recovery time between training sessions, and lack of variety in training can all contribute to the development of Achilles tendinopathy.
Biomechanical Factors
Footwear
Inappropriate or worn-out footwear can increase the risk of Achilles tendinopathy.
Shoes that do not provide proper support can lead to excess strain on the Achilles tendon.
Body Mechanics
Individuals with certain body mechanics may be more prone to Achilles tendinopathy.
This includes people with over-pronation (where the foot rolls inwards) or flat feet, which can increase strain on the tendon.
Medical Factors
Age
The risk of Achilles tendinopathy increases with age, as the tendon naturally loses flexibility and strength over time.
Sex
Achilles tendinopathy tends to be more common in men than in women, though the exact reasons for this disparity are not fully understood.
Underlying Medical Conditions
Certain medical conditions can increase the risk of developing Achilles tendinopathy.
For example, people with high blood pressure or diabetes are more likely to experience this type of injury.
Medication
Certain medications, such as antibiotics of the fluoroquinolone class, have been linked with an increased risk of tendon injuries, including Achilles tendinopathy.
Section Summary
While these non-genetic factors can increase the risk of Achilles tendinopathy, it’s important to note that the presence of these factors does not guarantee the development of the condition.
Many of these factors are modifiable, offering opportunities for prevention and management of Achilles tendinopathy.
Exercises Effective for Achilles Tendinopathy
Physiotherapy exercises, especially eccentric exercises (lengthening contractions), have proven effective in managing Achilles tendinopathy.
Examples of these include heel drops, calf raises, and toe walks.
These exercises aim to strengthen the calf muscles and increase the tendon’s capacity to manage the load.
How to Eat for Your Genes if You Have Achilles Tendinopathy
While there’s no “one-size-fits-all” dietary plan that suits everyone, research has begun to explore the interaction between nutrition and genetics in the context of health and disease, including Achilles tendinopathy.
Here, we consider a few genes that may influence dietary recommendations:
COL5A1 Gene
As discussed, the COL5A1 gene is involved in collagen production, a key component of tendons. Therefore, a diet that supports collagen synthesis may be beneficial.
Vitamin C, for example, is a crucial nutrient that aids in collagen formation.
It’s found in foods like citrus fruits, strawberries, bell peppers, and broccoli.
Proline, an amino acid found in meat, dairy, and eggs, also plays a role in collagen production.
Which COL5A1 gene variants do you have? Check your Ancestry DNA, 23andMe raw data
MMP3 Gene
MMP3 gene products are involved in the breakdown and remodeling of the extracellular matrix, which includes collagen.
Antioxidants may help moderate excessive activity of matrix metalloproteinases, potentially reducing tendon degradation.
Foods high in antioxidants include berries, dark chocolate, artichokes, and nuts.
Which MMP3 gene variants do you have? Check your Ancestry DNA, 23andMe raw data
IL-1β Gene
The IL-1β gene is involved in the inflammatory response, which can contribute to the pain and swelling associated with Achilles tendinopathy.
An anti-inflammatory diet may help manage these symptoms.
This could include foods rich in omega-3 fatty acids, which have potent anti-inflammatory effects.
These include fatty fish like salmon and mackerel, flaxseeds, and walnuts.
Which IL-1β gene variants do you have? Check your Ancestry DNA, 23andMe raw data
GDF5 Gene
Variants of the GDF5 gene may influence bone and cartilage development and repair.
Nutrients that support bone health, like calcium and vitamin D, could be beneficial.
Dairy products, fortified plant milks, leafy greens, and sunlight exposure for vitamin D can be helpful.
Which GDF5 gene variants do you have? Check your Ancestry DNA, 23andMe raw data
MTHFR Gene
Though not directly implicated in Achilles tendinopathy, the MTHFR gene, which plays a role in folate metabolism, is important for overall health and recovery from injuries.
Folate-rich foods like leafy green vegetables, legumes, and fortified cereals can help ensure adequate folate status.
Remember, it’s essential to speak with a healthcare provider before making significant dietary changes, especially if you have any underlying health conditions or are taking medication.
Which MTHFR gene variants do you have? Check your Ancestry DNA, 23andMe raw data
Summary
Q: What is Achilles tendinopathy? A: It’s a condition causing pain, swelling, and reduced function in the Achilles tendon due to overuse or repetitive strain.
Q: Can I run with Achilles tendinopathy? A: While possible, it’s not advisable without medical consultation as it may exacerbate the condition.
Q: How is Achilles tendinopathy treated? A: Treatment usually involves RICE, pain management, physiotherapy, and possibly surgery in severe cases.
Q: What causes Achilles tendinopathy? A: It’s primarily caused by overuse or strain, often seen in athletes or those participating in high-impact activities. Certain genetic and non-genetic factors also contribute.
Q: What exercises help with Achilles tendinopathy? A: Eccentric exercises like heel drops and calf raises can help manage the condition by strengthening the calf muscles.
References
- Alfredson, H., & Cook, J. (2007). A treatment algorithm for managing Achilles tendinopathy: new treatment options. British Journal of Sports Medicine, 41(4), 211-216.
- September, A. V., Schwellnus, M. P., & Collins, M. (2009). Tendon and ligament injuries: the genetic component. British Journal of Sports Medicine, 43(4), 241-246.
- Magnan, B., Bondi, M., Pierantoni, S., & Samaila, E. (2014). The pathogenesis of Achilles tendinopathy: a systematic review. Foot and ankle surgery, 20(3), 154-159.
- Maffulli, N., Sharma, P., & Luscombe, K. L. (2004). Achilles tendinopathy: aetiology and management. Journal of the Royal Society of Medicine, 97(10), 472-476.
- Habets, B., & van Cingel, R. E. H. (2015). Eccentric exercise training in chronic mid-portion Achilles tendinopathy: a systematic review on different protocols. Scandinavian journal of medicine & science in sports, 25(1), 3-15.
Written By
Share this article











