The Genetics of Type 2 Diabetes: Everything You Need To Know

Table of Contents
Type 2 diabetes (T2D) is a complex metabolic disorder characterized by high blood glucose levels due to insulin resistance or a lack of insulin production. This condition is influenced by a combination of environmental, lifestyle, and genetic factors. The genetic component of T2D has been a focus of research in recent years, with numerous genes identified that can increase susceptibility to this disease.
What is Type 2 Diabetes?
Type 2 diabetes is a condition that affects how your body uses sugar from the food you eat. Normally, your body breaks down food into a sugar called glucose, which is used for energy. The hormone insulin, produced by the pancreas, helps move this glucose into your body’s cells to be used as fuel.
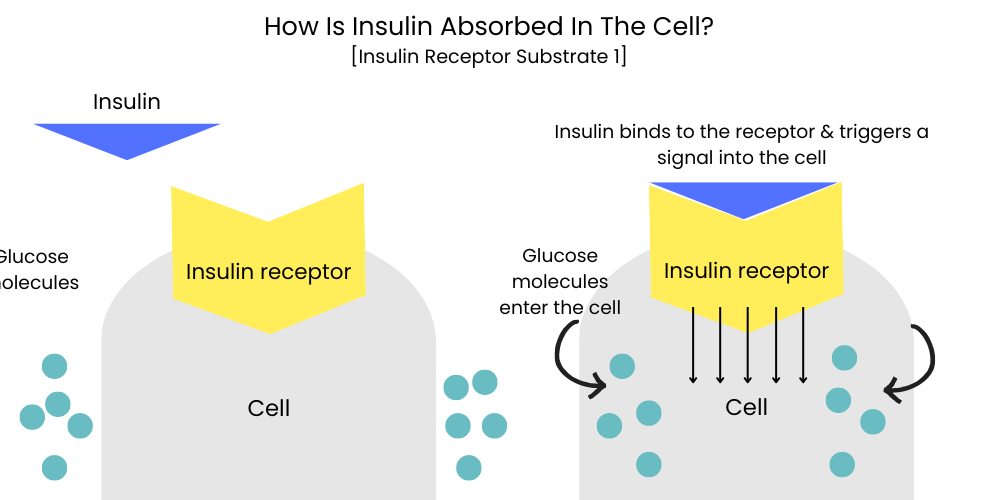
In T2D, your body either doesn’t make enough insulin, or it can’t use the insulin it does make properly. This is called insulin resistance. Because of this, the glucose can’t get into your cells easily, so it stays in your blood. This leads to higher than normal blood sugar levels, which over time, can cause serious health problems like heart disease, nerve damage, kidney disease, and vision problems.
It’s important to note that while T2D can be influenced by genetics, it’s also strongly linked to lifestyle factors like poor diet, lack of exercise, and being overweight.
What Causes Type 2 Diabetes?
T2D is a complex disease influenced by a range of factors. Here are the top five causes:
Overweight and Obesity
According to the World Health Organization, at least 80% of all type 2 diabetes cases are associated with overweight and obesity. The American Diabetes Association reports that people who are obese are 80 times more likely to develop T2D than those with a BMI less than 22.
Poor Diet
A diet high in processed foods, sugars, and unhealthy fats, but low in fiber can increase the risk of developing T2D. Studies suggest that consuming one to two servings of sugary drinks per day increases the risk of developing type 2 diabetes by about 25%.
Physical Inactivity
Lack of physical activity is a significant risk factor for T2D. According to a report by the Centers for Disease Control and Prevention, adults who are physically inactive have a 25-50% increased risk of developing type 2 diabetes compared to those who engage in regular physical activity.
Genetics and Family History
People with a family history of T2D are more likely to develop the disease. If one of your parents has type 2 diabetes, your risk of developing the disease is about 2 to 3 times higher than someone without a family history.
Age and Race
The risk of developing T2D increases with age, especially after 45 years. Additionally, certain racial and ethnic groups, including African Americans, Hispanic/Latino Americans, American Indians, and some Asian Americans, have a higher prevalence of type 2 diabetes.
Section Summary
It’s crucial to remember that while these factors increase the risk of T2D, they don’t guarantee that an individual will develop the disease. Many of these factors, such as weight, diet, and physical activity, can be modified to reduce the risk of type 2 diabetes.
Can Type 2 Diabetes Be Reversed?
Type 2 diabetes can often be managed and even reversed with lifestyle changes, particularly adopting a healthy diet, regular physical activity, and maintaining a healthy weight. While it may not be completely ‘cured’, many individuals with T2D can achieve normal blood sugar levels and maintain them without the need for medication. However, it’s crucial to remember that everyone is different and what works for one person may not work for another. Ongoing management under the supervision of a healthcare provider is essential.
What is the Difference Between Type 1 and Type 2 Diabetes?
Type 1 and type 2 diabetes are both conditions that cause high blood sugar levels, but they differ in their causes and management.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition, where the body’s immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. As a result, people with type 1 diabetes produce little to no insulin and must take insulin daily to manage their blood sugar levels. It typically develops early in life but can occur at any age.
Type 2 Diabetes
On the other hand, T2D primarily develops in adults and is associated with insulin resistance, where the body doesn’t use insulin effectively. Initially, the pancreas can compensate by producing more insulin, but over time, it can’t keep up, leading to high blood sugar levels. Type 2 diabetes can often be managed through diet, exercise, and medication.
Which is Worse: Type 1 or 2 Diabetes?
Neither type of diabetes is ‘worse’ than the other. Both type 1 and type 2 diabetes can lead to serious complications if not managed effectively, including heart disease, kidney disease, nerve damage, and vision problems. The key to preventing or managing these complications is maintaining good blood sugar control and leading a healthy lifestyle.
Is Type 2 Diabetes Genetic?
Yes, type 2 diabetes has a strong genetic component. Having a family history of type 2 diabetes can significantly increase an individual’s risk of developing the disease. Numerous genes have been associated with T2D risk. However, environmental factors, such as diet and physical activity, also play a crucial role in the development of type 2 diabetes.
The Genetics of Type 2 Diabetes
While lifestyle factors such as diet, exercise, and body weight significantly influence T2D, there’s also a strong genetic component. Having a family history of T2D can significantly increase an individual’s risk of developing the disease.
Studies involving twins and families have shown that when one identical twin has T2D, the other twin has a 70-90% chance of also developing the disease. Moreover, if both parents have T2D, their child has a 40% chance of developing it.
Key Genes Linked to Type 2 Diabetes
Several genes have been implicated in T2D, with variants in these genes potentially affecting insulin production and function, glucose metabolism, or increasing the risk of obesity. Let’s look at a few key genes:
TCF7L2 Gene
The TCF7L2 gene is thought to be the most significant T2D susceptibility gene discovered so far. Certain variations in this gene have been associated with an up to 80% increased risk of developing T2D.
KCNJ11 and ABCC8 Genes
The KCNJ11 and ABCC8 genes provide instructions for making parts of a protein found in the pancreas that regulates insulin secretion. Variations in these genes can affect the body’s response to insulin.
FTO Gene
The FTO gene is primarily associated with obesity, a significant risk factor for T2D. Certain variants in the FTO gene can increase the risk of obesity and thereby indirectly increase the risk of T2D.
Here is a sample SNP table representing a few key genetic variations associated with T2D:
| SNP ID | Gene | Risk Allele | Risk Increase | References |
|---|---|---|---|---|
| rs7903146 | TCF7L2 | T | Up to 80% | Grant SF, et al. |
| rs5219 | KCNJ11 | T | 20% | Gloyn AL, et al. |
| rs1801282 | PPARG | G | 25% | Altshuler D, et al. |
| rs9939609 | FTO | A | 20% | Frayling TM, et al. |
Non-Genetic Factors in Type 2 Diabetes
While genetics play a significant role in T2D, non-genetic factors such as diet, physical activity, and obesity are also important. Maintaining a balanced diet, regular physical activity, and healthy body weight can help manage T2D and may even help prevent it in those at high risk.
Recent Updates on Type 2 Diabetes Genetic Research
Research on the genetics of type 2 diabetes (T2D) is ongoing and continually evolving, offering new insights into the disease. Here, we highlight some of the most recent and significant updates in the field.
Discovery of New Risk Loci
Advances in genetic technologies, like genome-wide association studies (GWAS), have led to the discovery of new genetic risk loci (locations) for T2D. A recent study published in Nature Genetics in 2020 identified an additional 318 new risk loci associated with T2D, bringing the total number of associated loci to over 400. These discoveries give researchers a more complete picture of the genetic architecture of T2D.
Role of Gene-Environment Interactions
A growing area of research is exploring how genetic factors interact with environmental factors, like diet and physical activity, to influence T2D risk. One 2020 study found that a high genetic risk for T2D could be offset by a healthy lifestyle, further emphasizing the importance of environmental and lifestyle factors in disease risk and prevention.
Genetics of Diabetes Complications
Genetic research is not only focused on the risk of T2D but also its complications. Recent studies are looking into the genetics of microvascular and macrovascular complications, such as diabetic retinopathy, neuropathy, nephropathy, and cardiovascular disease. This line of research can help to identify individuals at high risk of complications and tailor their treatment accordingly.
Personalized Medicine Approaches
The ultimate goal of understanding the genetics of T2D is to improve patient care. This can be achieved through personalized medicine approaches, where treatment plans are tailored to an individual’s genetic makeup. This is an emerging area of research with promising potential to improve T2D management and outcomes.
Summary
-
What is Type 2 diabetes?
Type 2 diabetes is a metabolic disorder that leads to high blood sugar levels. It’s often associated with insulin resistance or a lack of insulin production.
-
What role do genes play in Type 2 diabetes?
Genes play a significant role in the development of T2D. Having a family history of Type 2 diabetes or certain genetic variations can increase an individual’s risk of developing the disease.
-
What are some key genes linked to Type 2 diabetes?
Some of the key genes linked to T2D include the TCF7L2, KCNJ11, PPARG, and FTO genes. Variations in these genes can influence insulin production and function, glucose metabolism, or obesity risk.
-
What non-genetic factors influence Type 2 diabetes?
Non-genetic factors such as being overweight or obese, having a poor diet, being physically inactive, as well as age and race, can significantly influence the risk of developing T2D.
-
What are the recent updates in genetic research on Type 2 diabetes?
Recent advances have identified over 400 genetic loci associated with T2D. Research is also delving into gene-environment interactions, the genetics of diabetes complications, and how personalized medicine approaches can improve patient care.
-
Can lifestyle changes help manage Type 2 diabetes?
Yes, adopting a healthy diet, regular physical activity, and maintaining a healthy weight can help manage and even reverse Type 2 diabetes in some individuals. However, ongoing management under the supervision of a healthcare provider is crucial.
References
- Grant SF, Thorleifsson G, Reynisdottir I, et al. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet. 2006;38(3):320-323.
- Gloyn AL, Weedon MN, Owen KR, et al. Large-scale association studies of variants in genes encoding the pancreatic beta-cell KATP channel subunits Kir6.2 (KCNJ11) and SUR1 (ABCC8) confirm that the KCNJ11 E23K variant is associated with type 2 diabetes. Diabetes. 2003;52(2):568-572.
- Altshuler D, Hirschhorn JN, Klannemark M, et al. The common PPARgamma Pro12Ala polymorphism is associated with decreased risk of type 2 diabetes. Nat Genet. 2000;26(1):76-80.
- Frayling TM, Timpson NJ, Weedon MN, et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science. 2007;316(5826):889-894.
- Mahajan A, Taliun D, Thurner M, et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat Genet. 2018;50(11):1505-1513.
Written By
Share this article












