Genetics of Familial Hypercholesterolemia: A Full Review

Table of Contents
Familial Hypercholesterolemia (FH) is a complex and crucial medical topic. This article will cover everything you need to know about FH, including its genetic makeup, inheritance patterns, diagnostic methods, and testing options.
What is familial hypercholesterolemia?
Familial Hypercholesterolemia (FH) is a complex genetic disorder with various aspects to consider. Below, we will break down this condition into different aspects to understand it more comprehensively.
Definition
Familial Hypercholesterolemia is an inherited condition characterized by significantly elevated levels of low-density lipoprotein cholesterol (LDL-C) in the blood. These high levels of LDL-C can lead to the development of fatty deposits in the arteries and the early onset of cardiovascular diseases.
Prevalence
FH is relatively common, affecting about 1 in 250 individuals globally. However, the disorder is often underdiagnosed, with estimates suggesting that only around 10% of cases are correctly identified and managed.
Symptoms
While FH itself might not present specific symptoms, the consequences of elevated LDL-C levels can manifest in various ways. Signs include:
- Fatty deposits (xanthomas) in the skin or tendons
- Cholesterol deposits (xanthelasmas) around the eyes
- Early development of coronary artery disease
- Chest pain or other symptoms of heart problems
Types
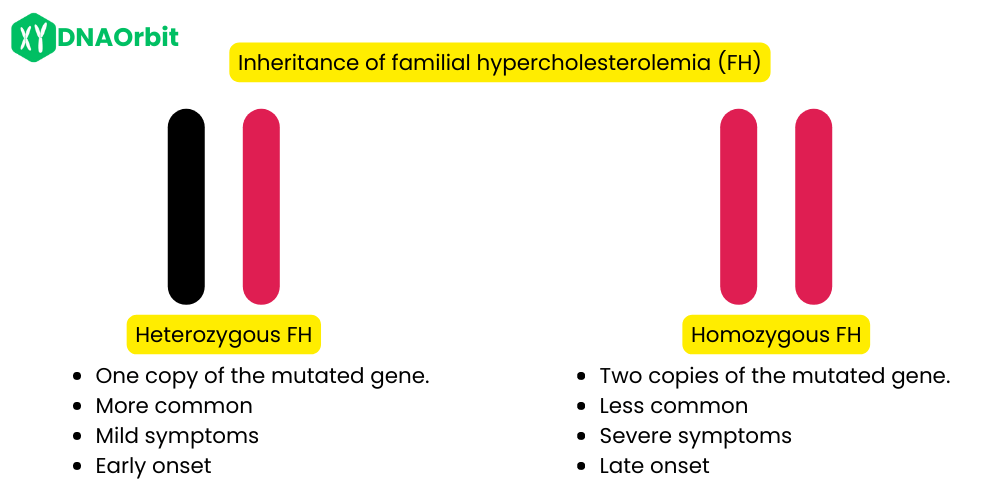
There are two main types of FH:
- Heterozygous FH (HeFH): One copy of the mutated gene is present. This is the most common form, with milder symptoms and later onset.
- Homozygous FH (HoFH): Both copies of the gene are mutated, leading to a more severe condition with earlier onset of symptoms.
Risk Factors
The primary risk factor for FH is having a family history of the disorder. Other factors that can exacerbate the condition include:
Complications
Untreated FH can lead to serious complications, mainly related to the heart and blood vessels. These include:
- Atherosclerosis
- Heart attack
- Stroke
- Peripheral artery disease
Treatment
Treatment for FH typically involves a combination of approaches:
- Lifestyle changes (healthy diet, exercise, etc.)
- Medication (such as statins to lower cholesterol)
- Regular monitoring and follow-up care
- In extreme cases, procedures like LDL apheresis may be required
Familial Hypercholesterolemia is a serious and potentially life-threatening condition if left untreated. Awareness, early diagnosis, and appropriate management are crucial to prevent its severe complications and provide those affected with a normal lifespan.
Is familial hypercholesterolemia dominant or recessive?
FH is an autosomal dominant disorder. This means that a person needs only one mutated copy of the responsible gene to have the condition. Offspring of a person with FH have a 50% chance of inheriting the mutated gene.
How is familial hypercholesterolemia inherited?
Being an autosomal dominant condition, FH is passed on to children from either parent. If one parent has FH, each child has a 50% chance of inheriting the gene mutation and the condition.
What is the cause of familial hypercholesterolemia?
Familial hypercholesterolemia is caused by a mutation in one of several genes that are responsible for the metabolism of LDL cholesterol. The most common mutations occur in the LDLR gene, which affects the LDL receptor’s ability to clear LDL cholesterol from the blood.
How to test for familial hypercholesterolemia?
Testing for FH includes a lipid profile blood test to measure LDL-C levels and genetic testing to identify mutations in the genes responsible for the condition. A medical history and physical examination may also be part of the diagnostic process.
How does familial hypercholesterolemia affect the body?
Familial Hypercholesterolemia (FH) has a profound effect on various systems within the body, particularly the cardiovascular system. Below, we explore the different ways this disorder impacts the body.
Elevated LDL Cholesterol Levels
FH leads to a significant elevation in low-density lipoprotein cholesterol (LDL-C) levels in the blood. LDL-C is often referred to as “bad cholesterol” because it can build up in the arteries and form fatty deposits.
Development of Atherosclerosis
The primary concern with FH is the development of atherosclerosis, where the fatty deposits form plaques within the arteries. These plaques can:
- Narrow the arteries, limiting blood flow
- Become unstable and rupture, leading to blood clots
Impact on the Heart
The narrowing and blockage of arteries directly affect the heart by:
- Increasing the Risk of Coronary Artery Disease: Reduced blood flow to the heart muscles can cause angina (chest pain) or lead to a heart attack.
- Heart Failure: Long-term effects of reduced blood flow can weaken the heart muscle, leading to heart failure.
Impact on the Brain
Reduced blood flow due to atherosclerosis also affects the brain by:
- Increasing Stroke Risk: Blockages can lead to a stroke if blood flow to part of the brain is cut off.
- Cognitive Impairments: Chronic reduced blood flow may cause cognitive impairments over time.
Impact on Peripheral Arteries
FH can also affect other arteries in the body, leading to:
- Peripheral Artery Disease: Narrowing of the arteries in the limbs, particularly the legs, can cause pain and mobility issues.
- Chronic Kidney Disease: Reduced blood flow to the kidneys can impair their function over time.
Impact on the Skin and Eyes
The buildup of cholesterol can lead to visible signs on the body, such as:
- Xanthomas: Fatty deposits under the skin, particularly around the joints and tendons.
- Xanthelasmas: Yellowish cholesterol deposits around the eyes.
Psychological Impact
Living with FH and the associated risks can have a psychological impact, including:
- Stress and Anxiety: Worrying about health and the need for ongoing treatment.
- Depression: Particularly if FH leads to limitations in daily life or chronic health issues.
Section Summary
Familial Hypercholesterolemia affects the body in multifaceted ways, primarily targeting the cardiovascular system but also having secondary impacts on other organs, the skin, and mental well-being. Early diagnosis and treatment are vital to mitigate these effects and help individuals with FH lead healthy life.
How is familial hypercholesterolemia diagnosed?
Diagnosis of FH involves a combination of clinical assessment, lipid profile testing, and genetic testing. A diagnosis is often made based on an LDL cholesterol level above a certain threshold, a family history of high cholesterol, and early onset of heart disease.
Is familial hypercholesterolemia genetic?
Yes, FH is a genetic condition caused by mutations in specific genes associated with cholesterol metabolism.
What are the five most prominent genes influencing familial hypercholesterolemia?
The most common genes associated with FH are:
- LDLR
- APOB
- PCSK9
- LDLRAP1
- STAP1
LDLR (Low-Density Lipoprotein Receptor)
LDLR is the most common gene associated with familial hypercholesterolemia. Mutations in this gene impair the LDL receptors’ ability to clear LDL cholesterol from the blood, leading to elevated cholesterol levels. Approximately 85-90% of diagnosed cases of FH are linked to mutations in the LDLR gene.
APOB (Apolipoprotein B)
APOB gene codes for apolipoprotein B-100, a protein that’s essential for the metabolism of fats, including cholesterol. Mutations in the APOB gene can lead to defective binding of LDL cholesterol to its receptor, causing elevated levels of LDL in the blood. This gene is responsible for approximately 5% of FH cases.
PCSK9 (Proprotein Convertase Subtilisin/Kexin Type 9)
PCSK9 is involved in the degradation of LDL receptors. Mutations in the PCSK9 gene can lead to reduced clearance of LDL receptors, thus increasing LDL cholesterol levels in the blood. This gene accounts for 1-3% of FH cases, and the discovery of its role has also led to new therapeutic interventions for high cholesterol.
LDLRAP1 (Low-Density Lipoprotein Receptor Adapter Protein 1)
LDLRAP1 plays a crucial role in the internalization of LDL receptors. Mutations in LDLRAP1 result in impaired functioning of LDL receptors, leading to elevated LDL cholesterol levels. Although rare, mutations in LDLRAP1 can cause a severe form of FH known as autosomal recessive hypercholesterolemia.
STAP1 (Signal Transducing Adaptor Family Member 1)
STAP1 is a more recently discovered gene associated with FH. While its precise role in cholesterol metabolism is still under investigation, mutations in STAP1 have been linked to high cholesterol levels in some patients. The exact percentage of FH cases attributed to STAP1 mutations is currently not well-defined, and more research is needed to understand its full significance.
SNP Table
Here’s a table that includes some well-known SNPs related to the five most prominent genes influencing familial hypercholesterolemia:
| Gene | SNP ID | Chromosome | Position | Effect |
|---|---|---|---|---|
| LDLR | rs688 | 19 | 11125579 | Affects LDL receptor function |
| APOB | rs1042031 | 2 | 21225809 | Associated with altered apolipoprotein B-100 |
| PCSK9 | rs11591147 | 1 | 55505625 | Increases LDL receptor degradation |
| LDLRAP1 | rs12095921 | 1 | 113607302 | Impairs LDL receptor internalization |
| STAP1 | N/A | 4 | N/A | Not well-defined, needs more research |
Please note that the SNP information provided is based on some well-known examples, and there are likely many more SNPs associated with these genes that can influence familial hypercholesterolemia.
Section Summary
These five genes represent a broad spectrum of genetic influences on familial hypercholesterolemia. The varying roles of these genes in cholesterol metabolism illustrate the complex nature of this disorder. Further research is essential to continue to unravel the mechanisms and potential therapeutic targets for FH.
Is there a genetic test for familial hypercholesterolemia?
Yes, genetic testing for FH is available and can identify the specific gene mutation responsible for the condition.
Does 23andMe test for familial hypercholesterolemia?
23andMe does not offer specific testing for familial hypercholesterolemia. It is advised to consult with healthcare providers for genetic testing options related to FH.
Summary
Q: What is FH? A: It’s a genetic disorder causing high LDL cholesterol levels.
Q: Is it dominant or recessive? A: Dominant.
Q: How is it inherited? A: It’s inherited in an autosomal dominant pattern.
Q: How to test for it? A: Blood tests, genetic tests, and clinical assessments.
Q: What genes are involved? A: LDLR, APOB, PCSK9, LDLRAP1, STAP1.
Q: Can I test for it with 23andMe? A: No, as of the last update, 23andMe does not test for FH.
References
- Goldstein, J.L., et al. “Familial hypercholesterolemia.” The Metabolic and Molecular Bases of Inherited Disease (2001): 2863-2913.
- Nordestgaard, B.G., et al. “Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population.” European Heart Journal 34.45 (2013): 3478-3490.
- Myant, N.B. “Familial defective apolipoprotein B-100: a review.” Journal of the Royal Society of Medicine 84.6 (1991): 341-344.
- Wald, D.S., et al. “Child–parent familial hypercholesterolemia screening in primary care.” The New England Journal of Medicine 375.17 (2016): 1628-1637.
Written By
Share this article











