What Is Ehlers-Danlos Syndrome & Is It Genetic?

Table of Contents
What is Ehlers-Danlos Syndrome?
Ehlers-Danlos Syndrome (EDS) is a group of connective tissue disorders characterized by a range of symptoms, including hypermobile joints, easily bruised skin, and a propensity for scarring. Below, we’ll dive into its definition, the role of connective tissue, types, and prevalence to give you a comprehensive understanding of the syndrome.
Definition and Overview
Ehlers-Danlos Syndrome is not a single condition, but a group of genetic disorders that primarily affect the connective tissues in the body. These tissues provide support to the skin, bones, blood vessels, and other organs. The syndrome was first described by two dermatologists, Edvard Ehlers and Henri-Alexandre Danlos, in the early 20th century.
The Role of Connective Tissue
Connective tissue is like the “glue” that holds the body together. It is made up of proteins, such as collagen, that provide structure and stability to the body’s various systems. In EDS, the connective tissue is faulty due to genetic mutations, leading to a range of symptoms that primarily affect the skin, joints, and blood vessels.
Types of Ehlers-Danlos Syndrome
There are 13 subtypes of EDS, each with its own set of symptoms and genetic causes. The most common types are the hypermobility type, classical type, and vascular type. While some types are milder, others like the vascular type can have serious complications including arterial rupture.
Prevalence and Demographics
Ehlers-Danlos Syndrome is relatively rare, affecting approximately 1 in 5,000 to 1 in 20,000 individuals worldwide. However, its actual prevalence may be higher due to underdiagnosis. It affects people of all genders and ethnic backgrounds.
Genetic Aspect
Most types of Ehlers-Danlos Syndrome are hereditary, meaning they are passed down from parents to their children through genes. Mutations in various genes, often those responsible for the formation of collagen, result in the different forms of EDS.
Section Summary
By understanding what Ehlers-Danlos Syndrome is, you can better grasp its complexity and the challenges it poses for those who live with this condition. The syndrome is diagnosed through a combination of clinical evaluation, family history, and, in some cases, genetic testing.
Do I Have Ehlers-Danlos Syndrome? A Short Quiz
- Do your joints extend more than normal?
- Do you bruise easily?
- Is your skin unusually elastic or smooth?
- Have you had multiple dislocations or sprains?
- Do wounds on your skin heal slowly or scar easily?
Download full detailed quiz here
How is Ehlers-Danlos Syndrome Diagnosed?
Diagnosis typically involves clinical evaluation, family history, and specific tests to measure skin elasticity and joint mobility. Genetic testing may be done to confirm the diagnosis, particularly for specific subtypes of EDS.
What are the Symptoms of Ehlers-Danlos Syndrome?
- Joint hypermobility
- Skin that is easily bruised
- Slow and poor wound healing
- Chronic pain
- Cardiovascular problems
How to Test for Ehlers-Danlos Syndrome?
The first step in testing for Ehlers-Danlos Syndrome (EDS) often involves a comprehensive clinical evaluation. This usually includes a thorough medical history, an examination of symptoms, and often a review of other family members’ medical histories. The healthcare provider may look for common symptoms such as hypermobility of joints, skin that bruises easily, or a history of dislocations and sprains.
Beighton Score for Joint Hypermobility
One common assessment tool used for initial evaluation is the Beighton Score, which measures joint hypermobility on a scale from 0 to 9. A score above a certain threshold may indicate hypermobility, one of the key symptoms of some types of EDS. However, the score is just one part of the diagnostic process and not sufficient on its own for a diagnosis.
Genetic Testing for Confirmation
If EDS is suspected based on the initial clinical evaluation, the next step is often genetic testing. This can include tests that look for specific mutations in genes commonly associated with EDS. It’s important to note that while genetic testing can confirm a diagnosis, it’s not available or necessary for all types of EDS. Consultation with a genetic counselor is often recommended both before and after testing.
Imaging and Other Diagnostic Tests
In some cases, additional diagnostic tests such as skin biopsies, echocardiograms, or MRIs may be used to assess the condition of various connective tissues and organs. These tests can be crucial for identifying symptoms that might not be immediately visible, such as cardiovascular issues associated with certain types of EDS.
Multidisciplinary Diagnostic Approach
Due to the complex nature of EDS, a multidisciplinary approach is often recommended for a thorough diagnosis. This may involve consultations with various specialists such as rheumatologists, cardiologists, and dermatologists, each evaluating for symptoms relevant to their field of expertise.
Section Summary
By incorporating multiple evaluation methods—from clinical evaluations to genetic tests and beyond—the chances of an accurate and thorough diagnosis are significantly improved. The sooner an accurate diagnosis is made, the sooner appropriate treatment and management strategies can be put into place.
Is Ehlers-Danlos Syndrome an Autoimmune Disease?
No, EDS is not classified as an autoimmune disease. It is a connective tissue disorder.
Is Ehlers-Danlos Syndrome Genetic?
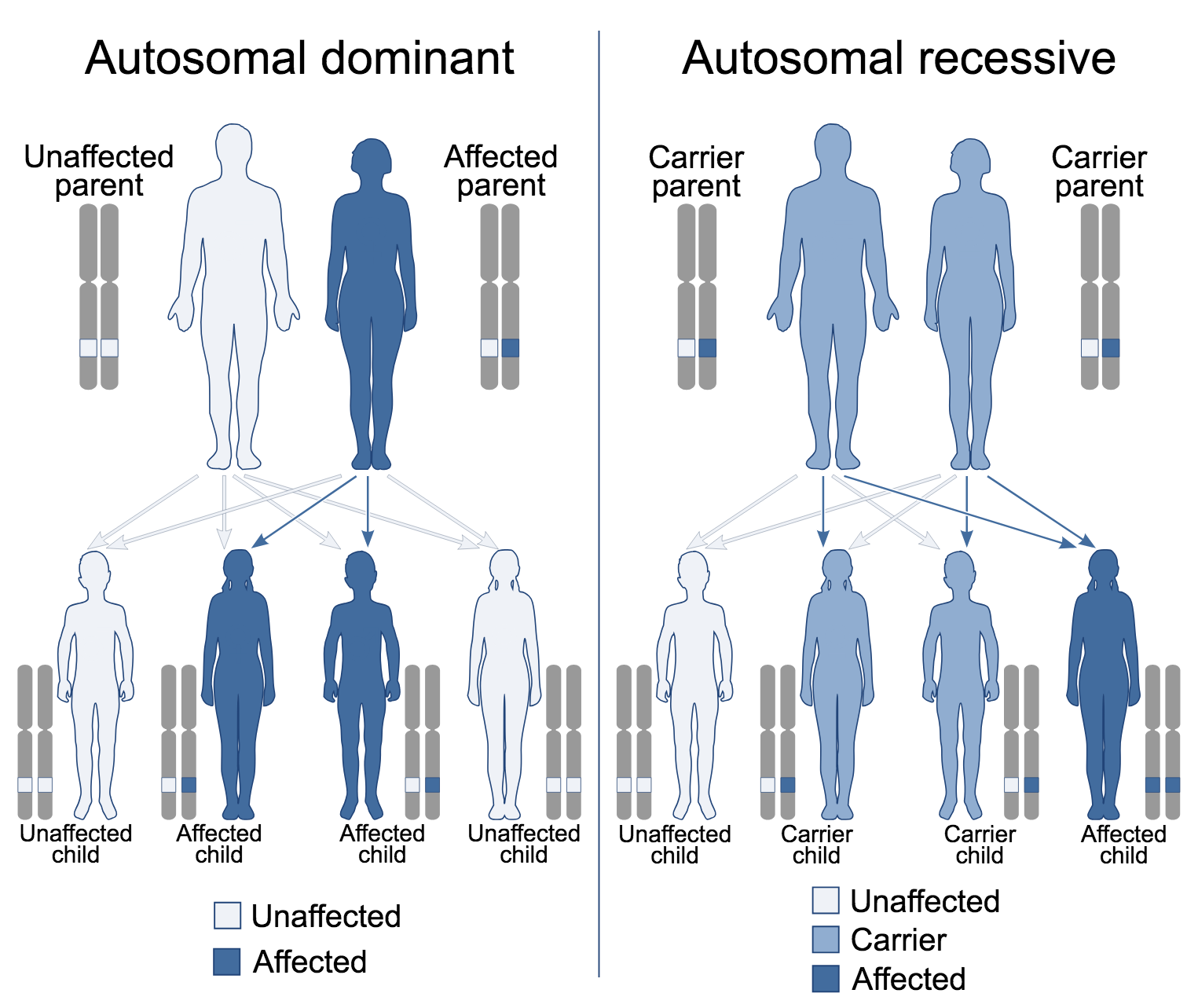
EDS is primarily considered a genetic disorder. Most types of EDS are inherited in an autosomal dominant or autosomal recessive manner, which means that the disorder can be passed down from one or both parents to their offspring. The genes associated with EDS are primarily responsible for the formation and function of connective tissues in the body.
Common Genetic Mutations Associated with EDS
There are specific genes commonly associated with the different types of EDS. These genes, such as COL5A1, COL5A2, and COL3A1, affect the structure, production, and processing of collagen—a key component of connective tissues. Mutations in these genes often lead to the symptoms commonly observed in EDS, such as skin that is easily bruised, hypermobility of joints, and other connective tissue anomalies.
Non-Genetic Factors
While EDS is largely genetic, there are also non-genetic factors that may influence the manifestation of the disorder. These may include hormonal changes, environmental factors, and even certain medications. However, these are generally considered secondary influencers and not primary causes of EDS.
The Importance of Genetic Testing
If EDS is suspected based on clinical symptoms, genetic testing is often the next step for diagnosis. This not only helps confirm the presence of EDS but can also help identify the specific type of EDS, which can guide treatment and management. Genetic counseling is often recommended for families where EDS has been diagnosed, particularly if planning for future children.
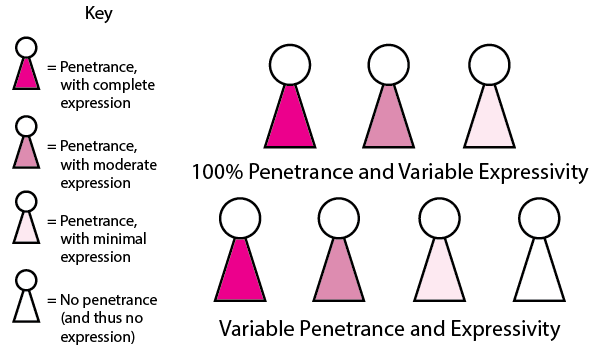
The Complexity of Penetrance and Expressivity
It’s important to note that even within families with a history of EDS, symptoms can vary widely in severity and presentation. This is due to concepts known as “penetrance” and “expressivity.” Penetrance refers to the likelihood that a person with a specific mutation will show symptoms, while expressivity refers to the range and severity of those symptoms. This adds another layer of complexity to the genetic nature of EDS.
By understanding the role of genetics in Ehlers-Danlos Syndrome, both patients and healthcare providers can make better-informed decisions about diagnosis, management, and even family planning.
What Are the Five Most Prominent Genes Influencing Ehlers-Danlos Syndrome?
The genetic factors underlying Ehlers-Danlos Syndrome (EDS) are complex and vary depending on the specific subtype of the condition. However, there are some key genes frequently associated with the development of EDS. Here, we explore the five most prominent genes that influence Ehlers-Danlos Syndrome.
COL5A1 and COL5A2: Classical EDS
These genes encode for type V collagen, a protein that helps provide structure and strength to connective tissues like skin, ligaments, and tendons. Mutations in either the COL5A1 or COL5A2 genes can lead to the classical type of EDS, characterized by highly elastic, smooth, and fragile skin as well as hypermobile joints.
COL3A1: Vascular EDS
The COL3A1 gene is responsible for encoding type III collagen, a protein that is especially important for the integrity of skin, lungs, and blood vessels. Mutations in this gene are linked to the vascular type of EDS, which is one of the most severe forms, with risks that include spontaneous arterial rupture and easy bruising.
TNXB: Hypermobile EDS
The TNXB gene encodes the tenascin-X protein, which plays a role in organizing the extracellular matrix that provides the structural framework for tissues. Mutations in this gene have been associated with the hypermobility type of EDS, characterized by extremely loose joints and chronic joint pain.
PLOD1: Kyphoscoliotic EDS
This gene is responsible for encoding the enzyme lysyl hydroxylase 1, which is crucial for the formation and stabilization of collagen fibers. Mutations in the PLOD1 gene lead to kyphoscoliotic EDS, a type of EDS marked by severe muscle hypotonia at birth, progressive scoliosis, and skin that scars easily.
ADAMTS2: Dermatosparaxis EDS
The ADAMTS2 gene produces a protein that aids in the processing of type I and type III procollagen molecules. A mutation in this gene is associated with Dermatosparaxis EDS, a very rare subtype characterized by extremely fragile and saggy skin.
Section Summary
Each of these genes plays a pivotal role in the manifestation and severity of different types of Ehlers-Danlos Syndrome. Understanding the genetic aspect can aid in accurate diagnosis and may eventually open avenues for targeted treatment strategies.
Does 23andMe Test for Ehlers-Danlos Syndrome?
23andMe does not specifically test for Ehlers-Danlos Syndrome, though it does provide some information on carrier status for a variety of conditions.
Summary
- What is EDS?
- A connective tissue disorder affecting skin, joints, and blood vessels.
- Is EDS Genetic?
- Yes, most types are inherited.
- How is it diagnosed?
- Through clinical evaluation, family history, and specific tests.
- Is it an autoimmune disease?
- No, it is not.
- Does 23andMe test for EDS?
- No, as of September 2021, it doesn’t.
References
Written By
Share this article